- Get link
- X
- Other Apps
- Get link
- X
- Other Apps
The Oral Microbiome & Its Impact on Every Other System in the Body - Dr Mark Burhenne
Every significant health website emphasizes the value of gut health in its headlines. Human health largely depends on the gut, and the diversity and population of the gut microbiome are key factors in determining gut health (also known as gut microbiota or gut flora). The mouth was referred to as "the mirror of health and disease in the body" by the US Surgeon General in 2000. There is no closed system here. Given how important gut health is to our understanding of health and disease and how closely the mouth reflects overall health, it should come as no surprise that gut and oral health are inextricably linked. This is where the oral microbiome is first understood.
What is the oral microbiome?
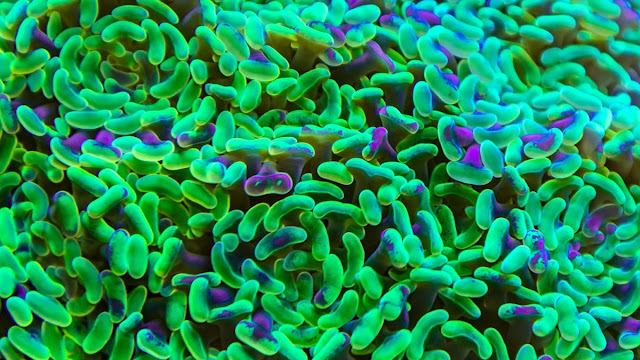
The oral microbiome, like the other three microbiomes of the body (gut, skin, and vaginal), is a group of bacteria that influences the development of health and disease. The tongue, the hard palate, the teeth, the region around the tooth surfaces, above the gums, and below the gums are just a few of the micro-environments in the mouth that are home to various bacterial populations. It serves as the first point of contact between the immune system, the environment, and the entire alimentary canal (the passage through which food travels through the body). This delicately balanced colony contains several hundred different species of bacteria (700+ have been identified as of this writing). The three other biomes also contain smaller populations than the most prevalent of these. The second most diverse biome in the body, after the gut, is the balance of bacteria in the oral cavity. Many of these (tooth decay, gingivitis, oral thrush, etc.) will manifest in the mouth, but they also significantly affect the gut and general health. The gut microbiota is colonized by bacterial populations from the mouth, according to a significant 2019 study published in the Journal of Oral Microbiology. This might affect immune responses and cause systemic diseases. This study specifically mentions the P. gingivalis bacteria as one that is present in the oral cavities and dysbiotic gut microbiomes of people with chronic gum disease (periodontitis). The mouth-body connection heavily involves the oral microbiome. Unfortunately, many dental care methods fail to recognize how crucial it is to maintain healthy oral flora. Instead, we are instructed to "clean" the mouth by disinfecting and sanitizing it. Let's examine how this biome may affect your digestive system and general health.How Oral Biome Diversity Impacts Gut & Overall Health?
I learned all about how oral diseases are brought on by oral bacteria during my training as a dentist. An excess of pathogenic (disease-causing) bacteria can result in a wide range of issues, including gingivitis, candida/oral thrush, and cavities. After speaking with ethnopharmacologist Cass Nelson-Dooley, MS, who has extensively studied the oral microbiome, I discovered that some of these problems may be related to the phenomenon known as "leaky gut." The oral equivalent of this is known as gingival epithelium permeability, although Cass has also affectionately referred to it as "leaky mouth" for many years, drawing attention to the clear connection to gut health. This permeability in the mouth is closely related to bacteria's ability to pass through the gums and into the rest of the body, similar to a leaky gut. Most research on it has been done in conjunction with diabetes, which is known to co-occur with chronic periodontitis. According to Cass' research, the gut contains 45% of the bacteria that are present in the mouth. Her most recent book, The Oral Microbiome, quotes: Every time you swallow, you introduce 140 billion bacteria, fungi, and viruses from your mouth into your digestive system each day. This is one of the reasons why extremely common oral diseases like cavities or gum disease are sometimes referred to as a "mismatch disease," similar to diabetes. This is so because, before the development of the modern diet, these diseases weren't widespread or even present. According to some experts, the modern, carb-heavy diet has a significant negative impact on the high rates of diseases because the evolutionary standard of our bodies is "mismatched" to modern diets. Below, I'll discuss dietary strategies to support the oral microbiome. But first: In many different ways, an oral infection can have serious effects on the body as a whole. These include systemic inflammation, infection of bacterial toxins that spread throughout the body, and bacteremia (the escape of bacteria through the gums to the bloodstream). Prevotella and Veillonella are two of the most significant bacterial communities in the oral biome that have the potential to negatively affect other aspects of health. Here are the major bodily organs and processes that are impacted by the state of your oral microbiome, starting with the digestive system.1. Gastrointestinal Tract:
Although gut dysbiosis (an imbalance of the microbiome) doesn't only cause GI tract issues, it can start wreaking havoc there.Inflammatory Bowel Disease:
IBS, Crohn's disease, and ulcerative colitis are the three conditions most commonly associated with the term "inflammatory bowel diseases," or IBD. One significant factor unites all of these illnesses: persistent, chronic inflammation. IBD may result from a variety of interactions, including genetic and epigenetic factors, immune reactions, and bacterial imbalances. However, the link between IBD and oral disease is one such factor that has drawn more attention recently. IBD patients frequently experience oral and dental symptoms like dry mouth, mouth ulcers, and pyostomatitis vegetans, a rare inflammation of the lips and mouth. Even though the research on the quality and diversity of the oral microbiome in people with inflammatory bowel diseases is somewhat limited, here is what we do know: 1- Streptococcus, Prevotella, Neisseria, Haemophilus, Veillonella, and Gemella are the predominant oral pathogenic bacterial species that are more prevalent in people with inflammatory bowel disease (IBD). 2- The oral microbiome is dysbiotic in IBD, which has inflammatory reactions. 3- When Klebsiella bacteria from the mouth colonize the gut, some strains cause the production of inflammatory TH1 cells. Only in a dysbiotic gut do these antibiotic-resistant bacterial strains typically colonize. In the context of a genetically vulnerable host, Klebsiella can "elicit a severe gut inflammation."Cirrhosis of the Liver:
Cirrhosis, a scarring of the liver, is frequently the result of liver diseases over time. The gut microbiome of people with liver cirrhosis is specifically dysbiotic. 54 percent of the problematic bacterial species in liver cirrhosis come from the mouth. The biomarkers that are used to identify these imbalances are very comparable to those found in patients with IBD and diabetes.Gut-Related Cancers:
Oral pathogens that cause tooth loss and advanced gum disease also raise the risk of gastrointestinal, pancreatic, and liver cancer. There are two reasons why this seems to occur. One, oral bacteria that enter the bloodstream or digestive system have the potential to cause systemic inflammation. Second, there is some evidence that they could trigger carcinogens that have been left in the mouth after drinking alcohol or smoking. Researchers have found that P. gingivalis and A. actinomycetemcomitans increase risk in the case of pancreatic cancer while Leptotrichia bacteria in the mouth reduce the risk. This starts to show how the oral microbiome affects not only the development of disease but also its prevention and general health.H. pylori:
Peptic (stomach) ulcers can develop in the stomach as a result of the Helicobacter pylori bacterial infection. Given that more than half of the world's population carries the H. pylori bacteria, infection with it is incredibly common. However, this bacteria can exist outside of the stomach as well. It's common to contract H. pylori again even after taking antibiotics to eradicate it. How? Particularly in those who have been identified as having H. pylori infection in the gut, H. pylori is extremely prevalent in the mouth. Your mouth may be the source if you experience recurrent H. pylori infection. Whether the bacteria enter the gut through "leaky mouth," bacteremia, or teeth cleanings, it is crucial to treat the infection from all angles if you want to completely eradicate it.2. Immune System:
It should come as no surprise that the gut microbiome has a significant impact on immunity given that your immune system is located there to an extent of at least 70%. But the mouth—the headwater of the entire digestive system—is where immunity starts. Many of the same bacteria that cause systemic disease today could have caused diseases in ancient oral microbiomes. Particularly, individuals with dental calculus (plaque) accumulation had weaker immune reactions to both systemic and oral diseases. Your body controls typical inflammatory processes in part through a healthy immune response. This delicate balance can be upset by pathogens in the oral cavity, which can also lead to chronic inflammation. These immune system disruptions can cause heart disease (which I will discuss below) and autoimmune conditions in addition to the immune responses you need to fight off the common cold and the flu. Particularly, oral microbiome dysbiosis is connected to the autoimmune disease rheumatoid arthritis. Interestingly, this study found that proper dental hygiene can partially reverse this dysbiosis. Oral microbiome health may also have an impact on HIV/AIDS cases. There is proof that untreated HIV/AIDS has a significantly different mouth biome diversity from healthy controls.3. Cardiovascular Health:
Atherosclerosis, which affects both the immune system and the gut, may have issues with the mouth's microbiome as a cause. The accumulation of plaque in the arteries can restrict the flow of nutrients and oxygen throughout the body. Periodontitis, an oral infection, and the risk of cardiovascular disease are closely related. Both of these have a very close connection to inflammation, both in the mouth and throughout the body.4. Gut-Brain Axis:
Scientific theory has a well-established place for the gut-brain axis. A healthy gut biome is essential to lowering your risk for brain and nervous system disorders, such as depression and Alzheimer's. The oral microbiome is a continuation of this axis, so oral health may have an impact on brain health by influencing the gut. Anxiety, depression, and Alzheimer's disease are a few examples of this.Alzheimer’s Disease:
The public has recently become aware of gingival bacteria as a possible cause of Alzheimer's disease. The bacteria that cause gum disease and Alzheimer's disease in the brain have a rare causative connection, not just a correlation, according to a ground-breaking study published in the early months of 2019. Although there is little information on how or why these two conditions are related, researchers have known for years that there is a connection between them. Additionally, scientists were able to create a gingipain inhibitor that, when administered to animal subjects, reversed the brain infection and saved neurons in the hippocampus in addition to lowering the risk for the disease. According to the theory underlying this association, P. gingivalis bacteria can travel from the mouth to the spinal cord and then on to the brain. Once it gets to the brain, it produces substances called gingipains that are directly correlated with the number of toxic tau tangles discovered in the brains of Alzheimer's patients.Anxiety & Depression:
The way the gut-brain axis affects anxiety and depression is a significant factor. When a newborn baby receives the mother's vaginal microbiota during delivery, this is thought to start as early as birth. The treatment of a dysbiotic gut is a necessary component of any effective depression or anxiety treatment. Sadly, the oral microbiome is frequently overlooked in this process. However, there is a clear link between anxiety/depression, tooth pain, bleeding gums, and poor dental health.5. Endocrine System:
The oral microbiome may have an impact on endocrine system diseases.Diabetes:
Diabetes is one of the "mismatch diseases" of modern life, as I already mentioned. Poor diet and lifestyle choices, such as being sedentary or being exposed to toxins in the home, are closely related to it. But once periodontitis sets in, an inflammatory condition that is itself brought on by a dysbiotic oral microbiome, the risk of diabetes skyrockets. Diabetes significantly alters the oral biomes of diabetics compared to non-diabetics. It's still unclear whether the dysbiosis of the gut and oral microbiomes or the onset of diabetes occurs first, but it appears to be a two-way process.
Adverse Pregnancy Outcomes:
Adverse pregnancy outcomes (APOs) include problems with pregnancy in birth, including: - Preterm labor. - Preterm membrane rupture. - Preeclampsia. - Miscarriage. - Intrauterine growth retardation (a major growth issue connected to fetal morbidity and some congenital anomalies). - Low birth weight. - Stillbirth. - Neonatal sepsis. F. nucleatum is the oral bacteria that are most frequently linked to these APOs. It has been discovered in fetal and placental tissues following many of the aforementioned conditions. This occurs when the mother's periodontal disease causes the bacteria to spread from her mouth to the placenta and fetus. Potential tissue damage and unsatisfactory fetal development are brought on by inflammation and dysfunctional immune responses. Some of these unfavorable pregnancy outcomes may also be caused by P. gingivalis and Bergeyella bacteria. Researchers anticipate that by identifying these widespread pathogens, earlier and more precise diagnosis will aid in risk screening.Obesity:
Although many different factors contribute to obesity, a 2009 study may have identified a root cause in the oral microbiome. In comparison to the control group, saliva from more than 98 percent of the obese women in the study contained very high levels of the bacteria Selenomonas noxia. We are unable to draw a cause-and-effect conclusion from this study. For instance, because their diets are so high in starchy carbohydrates and sugar, many obese people have dietary patterns that dysregulate the oral microbiome. The fact that so many of the subjects shared a specific pathogen, however, warrants further investigation.Polycystic Ovarian Syndrome (PCOS):
In the developed world, PCOS, an endocrine disorder that affects up to 21% of women of childbearing age, is thought to be the most typical reason for infertility.
The health of the gut microbiome has a direct bearing on this condition. Particularly, Prevotella bacteria are thought to play a role in polycystic ovarian syndrome.
Recognize those microbes? You should because it is a typical oral pathogenic bacterium that is also present in the gut.
In a 2016 study, Prevotella was found in excess in the saliva of women with PCOS, showing up at higher levels than any other bacterium.
6. Nitric Oxide Production:
Nitric oxide supports the body's natural repair processes in both the mouth and body. It affects organs from the gut to the brain and can reduce insulin resistance, blood pressure, digestion, cancer risk, and chronic inflammation. Nitric oxide production declines when there are lots of "nitrate-reducing bacteria" in the oral microbiome. This increases the risk of high blood pressure and other heart diseases, among other issues that can arise throughout the body.High-Sugar Diets: Bad for the Gut & Mouth
The findings are crystal clear when it comes to a diet to support the gut and oral microbiomes: breaking our sugar addiction is essential. Three factors make eating a lot of sugar and other starchy carbohydrates bad for bacterial health: 1- Increased inflammation is the result, and this has a significant impact on the entire body (often beginning with the mouth and gut). 2- Regular sugar consumption causes the pH in the mouth to become more acidic. The demineralization of teeth is influenced by an acidic environment. 3- Plaque accumulation from diets high in carbohydrates causes the oral microbiome to become dysbiotic, which worsens conditions like heart disease and cavities. The pH of the mouth is altered by poor oral hygiene, a high sugar intake, and insufficient salivation. This favors the growth of particular bacteria that thrive in acidic environments and produce acid, further lowering the pH and raising the risk of tooth decay. However, although oral hygiene practices are frequently discussed, diet is usually the most significant factor on this list. Overall, it creates an acidic environment with less bacterial diversity where S. mutans can flourish and non-pathogenic Streptococcus dies out. S. mutans and yeast take over in an environment that is more acidic, eventually leading to dental caries. Although the term "dysbiosis" isn't used in the literature about oral health, the microbial imbalance in the mouth that leads to the emergence of dental caries unquestionably falls under the category of dysbiosis. Unlike modern man, paleolithic people did not require probiotic supplements or dental cleanings. All of this stems from the fact that a Paleo-centric diet is rich in fruits, vegetables, healthy fats, non-farmed animal proteins, and limited in carbohydrates. Another sign of a systemic sugar problem is oral thrush, also known as candidiasis of the mouth. Candida overgrowth is best treated with a multi-system approach that always starts with eliminating sugar and also includes other treatments like glutamine rinse, chewable CoQ10, vitamins and minerals to support immune function, and oral and gastrointestinal antibiotics.Pregnancy, Birth, and the Microbiota:
One of the first questions I ask brand-new patients is one that frequently causes them to raise an eyebrow: "How were your birth and early years?" I'm curious about: - If they were breastfed as a baby, and- if they were delivered vaginally or by C-section
These inquiries are important because the diversity of your microbiome (all four of them!) starts before conception and lasts the rest of your life. Early in pregnancy, a developing fetus begins to inherit the body's bacterial ratio health.
The infant's microbiomes are passed on during vaginal delivery. According to a 2011 study, this has a particular impact on the diversity of the oral microbiome as well as the other two to three (depending on gender).
Even though C-sections are sometimes necessary and are great for risky deliveries, losing the biome is a big deal. It is well known to raise the risk of gastrointestinal and general health problems like celiac disease, asthma, type 1 diabetes, and obesity. One oral pathogen, Slack exigua, is only present in newborns who were delivered via C-section.
Vaginal microbial transfer, a more recent technique, has been suggested as a helpful remedy for restoring microbiota to infants born via Caesarean.
Additionally, breastfeeding affects how the oral microbiome develops. The oral and gut microbiomes of the nursing infant continue to develop with the assistance of the mother's microbiota during this time.
The answers to these inquiries help me establish a baseline for what to anticipate from my patient's oral biome, even though not every mother can or even chooses to breastfeed. This will enable me to give them advice on how to support their oral microbiome and enhance their dental and general health as a result.
7 Ways to Support Your Oral Microbiome:
There are several ways to support the health of your oral microbiome in addition to your birth and breastfeeding experiences. By extension, this can contribute to a healthier body as a whole!1. Reset Your Diet:
By regulating the biofilm on your teeth and lowering plaque buildup, many foods promote oral health. Here are some general "dos" and "don'ts" regarding these dietary changes, which can become complex: Do… 1- Consume foods high in minerals, such as leafy greens, grass-fed dairy, and premium seafood. 2- Get a lot of good fats, such as grass-fed butter or ghee, fatty fish, nuts, and healthy oils (coconut, avocado, and olive oils are excellent places to start). Also, eat fatty portions of grass-fed meat. 3- Include as many non-starchy vegetables as you can in your diet. 4- Consume foods high in vitamin K, such as grass-fed butter, pastured eggs, and chicken liver. 5- To keep your mouth and body well-hydrated, consume a lot of water. 6- To help your teeth remineralize with xylitol, think about chewing sugar-free gum (but be careful, as it is toxic to cats and dogs). Don’t… 1- More than 15% of your plate should be made up of carbohydrates. White bread, pasta, rice, crackers, and similar foods are the worst for your bacterial diversity. Although complex carbohydrates don't do much better for your teeth than refined ones, they can still be consumed in moderation. 2- Consume desserts, cookies, or other sweets every day. In exchange for a lot of calories and, more worrisome, sugar compounds that can disrupt your biome in just one day, these treats provide very little nutrition. 3- Long-term consumption of soda, fruit juices, coffee, kombucha is encouraged. Even though drinking coffee and kombucha throughout the day has some positive health effects, it also promotes demineralization. If you choose to drink one of these things, try to limit your time to 20 to 30 minutes and then brush roughly 45 to 60 minutes later. 4- Use too much phytic acid. Rice, beans, and other grains and legumes are high in phytic acid, which can affect the oral microbiome.2. Start to Mouth Taping:
I've already mentioned this, but a dry mouth is an ideal environment for bacterial overgrowth. It might even be a bigger cause of cavities, gum disease, and bad breath than diet, in my opinion! You can significantly reduce dry mouth issues by mouth taping at night to stop breathing through your mouth. This will maintain the health of your biome and lower your risk of developing oral, gastrointestinal, and general diseases.3. Brush and Floss Regularly:
Brushing and flossing are essential for managing oral biofilm and the oral microbiome, especially for those who continue to consume a standard Western diet. I advise brushing and flossing as soon as you wake up, right before bed, and 30-45 minutes after a meal high in carbohydrates.4. Don’t Skip Your Cleanings:
In an ideal scenario, a patient could avoid dental cleanings for 12 to 18 months if they followed a strict Paleo or ketogenic diet. But very few individuals—my own family included—have the motivation or capacity to adhere to a strict diet that religiously. Teeth cleanings every six months are crucial to maintaining a healthy oral microbiome for this reason. If your hygienist doesn't remove the plaque buildup, it might promote the pathogenic oral bacteria's dysbiotic growth.5. Scrape Your Tongue:
In the course of dental hygiene practices, the tongue is occasionally forgotten. But there's an easy fix—just start scraping your tongue. It's simple, inexpensive, and quick to form the habit of scraping your tongue to get rid of bacteria buildup on the tongue. Even the taste of your food and bad breath can be improved by it!6. Ditch the Conventional Mouthwash:
It seemed pretty obvious to me after learning so much about the value of having a healthy variety of bacteria in the mouth that killing "up to 99.9 percent of oral germs" isn't a good idea. Antibiotics are to the gut microbiome what conventional mouthwashes are to the oral microbiome. A very bad case of the overgrowth of one or two bacterial strains can occasionally be eliminated, leaving you with a "clean slate." However, alcohol-based mouthwash also dries out the mouth when used frequently in addition to removing your mouth's natural defenses against oral disease. Try making your mouthwash or using a natural brand that supports the mouth's microbiota as an alternative.7. Try Oil Pulling:
Oil pulling, unlike mouthwash, is a fantastic habit that encourages microbial diversity in the mouth while reducing inflammation, particularly if you use coconut oil. I advise oil pulling for just 1-3 minutes every morning rather than 20 minutes per day. Just keep in mind to spit the oil into the trash rather than the sink because, as it re-hardens, it can clog pipes.Key Takeaways: The Oral Microbiome:
As we can see, the oral microbiome and, indirectly, the health of the entire body are closely linked. You can promote oral and general health by promoting a healthy microbiome as opposed to eradicating bacterial diversity with traditional antiseptic treatments (like mouthwash).
bad bacteria
bad breath
dental care
gum disease
gums health
healthy teeth
mouth bacteria
Oral Microbiome
prodentim
ProDentim reviews
ProDentim reviews 2022
teeth health
tooth decay
- Get link
- X
- Other Apps



Comments
Post a Comment